Total Health Blog | The future of health is here
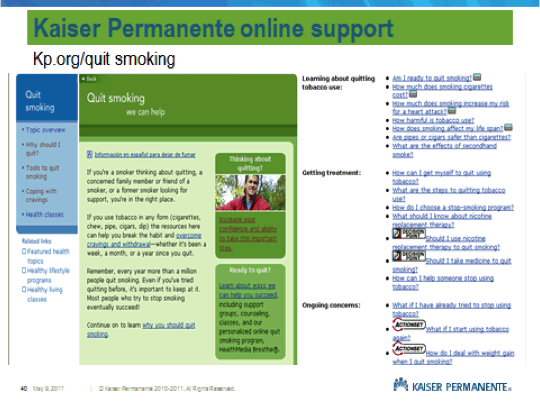
Just Breathe… Smoking Cessation Support
While it is difficult to overcome the addiction of smoking and completely kick the habit,…
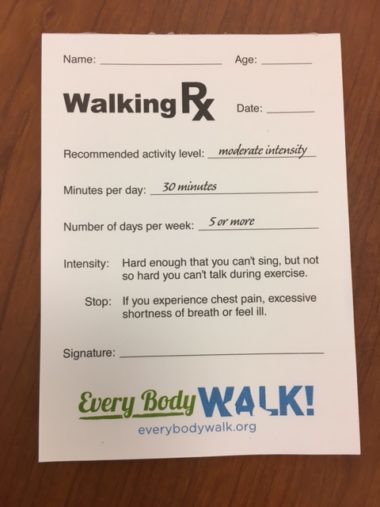
Exercise as a Vital Sign
Since May is National Physical Fitness and Sports Month, we were reflecting on a meeting…
New Perinatal Depression Display
Perinatal depression occurs in 12-20% of all pregnancies and can include premature delivery, decreased maternal-child…
A Future of Health Care Without Walls
Today, May 10, at the Kaiser Permanente Center for Total Health, the Network for Excellence…
Nurses Week 2017
National Nurses Week is May 6 to 12. It's a time to honor, celebrate and…
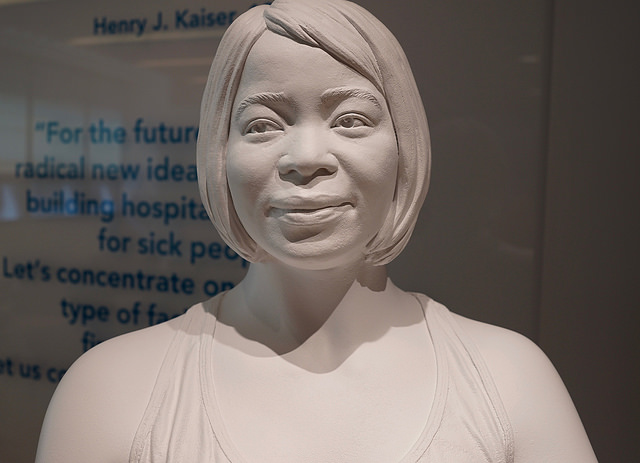
Nursing Leadership Now On Display
https://www.flickr.com/photos/taedc/34106560582/in/album-72157682858595535/ In November 2016, I had the distinct (and long sought after) honor of meeting…
Q&A with Kaiser Permanente Chairman and CEO Bernard Tyson on Mental Health
Kaiser Permanente Chairman and CEO Bernard J. Tyson discussed mental health, the social determinants of…
Kaiser Permanente Launches ‘Find Your Words’ Campaign to Fight Stigma Around Mental Health
Kaiser Permanente’s “Find Your Words” public health awareness campaign focuses on TV, radio and online…
Four Ways the Health Care Industry Can Help Green the Planet
Earth Day 2017 is April 22, a good time to consider the many ways both…
Why Talking About Depression Is a Radical Act
Depression is a topic that remains shrouded in silence, yet it’s a condition that has…
Tapping the Power and Potential of Technology Together
Digital technology is revolutionizing our world in ways we are only beginning to realize. Recently…
Taking Bids on Hospital of the Future
As Silicon Valley’s main hospital system and insurer, KP has been working with tech companies…
Virtual Care Lets Physicians Provide Care Anytime, Anywhere
The world of health care is changing. Telehealth options such as video visits, phone visits,…
The Future of Care Delivery
You walk in, verify at a kiosk that you’ve already checked in and paid, plug…
New resource to help identify and address social and non-medical needs
Today marks the launch of the Social Interventions Research & Evaluation Network (SIREN) website, a new…
What’s the Outdoor Industry’s Role in Healthcare Reform?
What's the Outdoor Industry's Role in Healthcare Reform? An article recently published by RootRated.com, explores…
Germ-free flying
It's Spring Break and you’re about to board a metal tube flying 40,000 feet above…
When Conventional Wisdom Becomes Outdated: How new perioperative guidelines can save time, pain, and cost
Maurice Cates, MD, is an Orthopedic Surgeon at Kaiser Permanente's Fredrick Medical Center. He is the chief…
Taking Predictive Analytics to the Next Level
Using Predictive Analytics in health care holds huge promise for improving care quality and outcomes…
Hospitals target nutrition, other social needs to boost health
Kaiser Permanente's Nirav Shah, MD, MPH, spoke with USA Today about the social determinants of…
Healthy Meeting’s Tip – Red Wine & Chocolate Bites
According to The Heart Foundation, February has been designated at Heart Health Month. Heart disease…
What Women Need to Know About Heart Disease
A stomach ache, jaw pain, fatigue. Each symptom on its own may not prompt…
Consumer Driven Models can Transform Care
Healthcare IT News interviewed Kaiser Permanente CIO Dick Daniels and he shared his perspective on Kaiser…
Defining Success In Resolving Health-Related Social Needs
A recent Health Affairs blog offers a perspective on the challenges of addressing the social…
Sticking to our New Year Resolutions
The Center for Total Health team -- and extended staff members -- have kicked off…
Strengthening Medicaid as a Critical Lever in Building a Culture of Health
The National Academy of Social Insurance (NASI) hosted its annual membership meeting and reception at…
NBA and Kaiser Permanente to Host Second Annual Total Health Forum
The National Basketball Association and Kaiser Permanente, will hold the second annual Total Health Forum…
Honoring National Diabetes Month and World Diabetes Day
In honor of National Diabetes Month and World Diabetes Day, we wanted to highlight important…
Fighting Hunger During the Holiday
We know that “total health” is about more than absence of sickness, it’s about having…
The dirty truth about receipts
Guest blogger Joel Sigler is senior manager for Kaiser Permanente National Environmental, Health & Safety…
Physician Leadership in the Movement Toward Accountable Care
Blog by Elizabeth Keating Senior Project Manager, Council of Accountable Physician Practices "It will not…
Health Care Topics Candidates Ought to Discuss
Dr. Robert Pearl, MD, Chairman and CEO of The Permanente Medical Group and the Mid-Atlantic…
Can you see me now? Video Visits at Kaiser Permanente
Dennis Truong, MD, is an emergency medicine specialist and the telemedicine director for the Mid-Atlantic…
Why You Should Reflect on Your Health This September
When was the last time you reflected on your total health journey? From your childhood…
I Want To Be The Next Summer Intern!
This summer, I interned at the Center for Total Health through the Kaiser Permanente Mid-Atlantic…
This Week in Total Health: Sweating the Details
Another busy week has drawn to a close at the Center for Total Health. On…
How do you measure a WELL building? Our Preliminary Audit
https://www.flickr.com/photos/138471261@N07/28859673656 We've completed our preliminary audit on the way to full WELL (@WELLCertified) certification. The WELL…
Mayor, What Will You Do To Improve My Health?
On July 19, Smart Growth America (@SmartGrowthUSA) hosted its annual Local Leaders Council (@SGALocalLeaders),meeting at the Center…
Week in Total Health: All About the Future
The week of July 18 was a busy one for the Center for Total Health,…
Transgender Health Meet and Greet
In 2013, we hosted a first conversation, the Transgender Health Care Dialogue. In 2016, we hosted…
This Week in Total Health: It’s All About Care
Another busy week wraps up at the Center for Total Health. We welcomed inspiring visitors…
Vision Zero for Who? #MoveEquity chat
What opportunities exist to create safer, more equitable streets and neighborhoods? How can law enforcement be…
National HIV Testing Day
For National HIV Testing Day, we offer this following post written by community practitioners, advocates, activists and…
This Week in Total Health: Building for Health
This week, the Center for Total Health met with people designing for total health, whether…
Don’t Let a Failing Heart Relegate You to Endless Doctor and Hospital Visits
Dr. Ameya Kulkarni is an interventional cardiologist with the Mid-Atlantic Permanente Medical Group. No one…
Better Together Health, with Council of Accountable Physician Practices
https://www.flickr.com/photos/138471261@N07/27729858495 Innovations in chronic care were featured in the Council of Accountable Physician Practices (CAPP)…
Hepatitis C: It’s Curable, So Let’s Find the People who Need to be Cured
Dr. Michael Horberg is Executive Director Research, Community Benefit and Medicaid Strategy of the Mid-Atlantic…
Preview: Better Together Health Returns to CTH
Next week, the Council of Accountable Physician Practices (@accountableDOCS) will host the second in a series…
Two Weeks in Total Health: We’ve Been Busy!
The week of May 16 kicked off with a two-day Ragan Public Relations (@RaganComms) Measurement Summit. One of…
Help Us Write Our Veteran’s Story
On Memorial Day, we recognize and honor our fallen soldiers, those who have made the…
Bike to Work (or Lunch) Day 2016
Across the country, bike commuting grew 62% from 2000 to 2014. Washington, DC is among…
This Week in Total Health: Keeping it in the KP Family
This week, the Center for Total Health team got to spend time with hundreds of…
First Mother’s Day Without Mom
Patti Harvey, senior VP, Medicare Clinical Operations and Population Care, and executive director, Care Management…
This Week in Total Health: Championing the Future
As we tend to do, we hosted leaders who look ahead. The Accelerated Leadership Development…
CEO Roundtable Policy Summit 2016
On April 29, the Kaiser Permanente Center for Total Health hosted a policy summit…
Paving the Way to Active, Sensored Streets: Part 2
Our guest blogger this week is Sam Piper, Senior Planner, Alta Planning + Design. Alta Planning + Design…
Paving the Way to Active, Sensored Streets: Part 1
Our guest blogger this week is Sam Piper, Senior Planner, Alta Planning + Design (@altaplanning). Alta Planning +…
Health Care That Targets Unmet Social Needs
Targeting the social determinants of health is a critical piece in improving an individual's overall well-being…
This Week in Total Health
This week, the Center hosted a three day private board meeting, so we're a little…
Employers As Innovation Partners
Earlier this month at the Center for Total Health, Kaiser Permanente invited members of its…
National Healthcare Decisions Day Today!
Check out this great video on a few short steps you can do for yourself today!…
This Week in Total Health: The End of an Era
As another busy week comes to a close at the Center for Total Health, our…
National Healthcare Decisions Day: April 16
In recognition of National Healthcare Decisions Day on April 16, Christina Kerby, a senior communications consultant with…
Even in Health, Money Talks
Last November, the Center for Total Health commissioned a survey exploring the factors that comprise total health,…
Five Years of Total Health
On Monday, the Center for Total Health celebrated its 5th birthday. So much has happened…
This Week in Total Health: The Many Faces of Innovation
It can be easy to think of innovation as technology and gadgets, but this week…
This Week in Total Health
Another great week at the Center for Total Health! We were thrilled to meet with…
This Week in Total Health: Service
This had to be the photo for This Week in Total Health. https://www.flickr.com/photos/138471261@N07/25602134192/ It's of…
Palliative Care Promotes Quality of Life for those with Advanced Illness
For those living with an advanced illness, the stress of having to discuss difficult topics…
This Week in Total Health: In Motion
The visitors to the Center for Total Health this week came from the future, to…
A year of tracking on a complete street: The Metropolitan Branch Trail
The Center for Total Health just marked its one year anniversary of population sensing on…
This Week in Total Health: Lots to Learn
The visitors to the Center for Total Health this week had a lot to teach us. They…
This Week in Total Health: An International Affair
This week, the Center for Total Health was honored to host a delegation from the…
Serving the needs of children and adolescents who have experienced sexual violence
Guest blog post by Marcy Levy, Senior Technical Advisor, JSI Research and Training Institute, Inc…
This Week in Total Health: Tours Rule
This week, we were delighted by a surprise visit from James Hamrick, MD (@HJamesHamrick), an oncologist…
Addressing Autism – Understanding a Complex Condition
Autism spectrum disorder (ASD) is a developmental disorder that the CDC estimates affects one in…
This Week in Total Health: Maintenance Rules
Last week, the Center was closed to the public to allow for upgrades to our…
This Week in Total Health: Innovation and Transportation Rule the Week
After being closed to the public for a few weeks for maintenance work, the Center…
Health Care as Part of the Climate Problem and Part of the Climate Solution
Hospitals and health systems, particularly in the most industrialized settings, make a significant impact on…
Growing Numbers of Clinics Ask about Physical Activity along with Taking Your Pulse
Everyone knows walking is good for you. It’s plain common sense, backed by a wealth…