 Michelle, 55, an African American Kaiser Permanente member in Southern California, was disheartened when she learned that she had high blood pressure. But her outlook changed with the encouragement of her doctor who worked with her to develop a diet and exercise regimen.
Michelle, 55, an African American Kaiser Permanente member in Southern California, was disheartened when she learned that she had high blood pressure. But her outlook changed with the encouragement of her doctor who worked with her to develop a diet and exercise regimen.
Michelle was grateful for the support.
“Even in my visits when I started the weight loss, she was very encouraging,” she said. “That makes you want to lose a little more and do the best you can. I think that I started doing some of these things so by the time I came back she would notice a difference.”
Michelle has successfully reduced her blood pressure, lost over 20 pounds, and built a sustainable, healthy lifestyle.

African Americans consistently have lower rates of hypertension control than whites, a higher prevalence of high blood pressure, and are more likely to develop hypertension at a younger age. In addition to genetic, environmental, social, and lifestyle factors, researchers believe that disparities in health care quality are driving these differences.
A new Kaiser Permanente Policy Story from the Institute for Health Policy highlights recent measures implemented in Kaiser Permanente facilities to treat African American patients with hypertension. It discusses how these efforts have led to improved care through increased access, better patient/provider communication, support in lifestyle changes, practice of evidence-based medicine, and use of health information technology (HIT).
Another effort is a $2.55 million grant to the American Heart Association Initiative to address high blood pressure among African Americans in two U.S. cities (Atlanta and San Diego) over three years. The program will depend upon community-based efforts to track blood pressure readings between community clinic workers, volunteer health mentors, doctors, and patients to create a model that can be replicated in communities across the country.
Another Kaiser Permanente initiative known as “ALL/PHASE” – that includes the use of three low-cost medications to reduce heart attacks and strokes – is aimed at reducing disparities in cardiovascular disease among low-income diabetics over the age of 50.
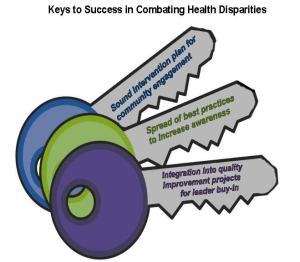
“It takes awareness and community engagement, gaining buy-in from leaders, integrating disparities work into quality improvement projects, and spreading best practices,” said Murray Ross, PhD, vice president with Kaiser Permanente and director of the Institute for Health Policy. “An increased focus on health disparities will help to reduce the occurrences of health inequities and inequalities, ensuring that all patients receive high quality health care.”