Last week at HIMSS in New Orleans, one of the booths that captured our attention was that of Archimedes, a company focused on bringing quantifiable analysis to health care. The folks from Archimedes were at HIMSS to talk about their product, IndiGO – which stands for Individualized Guidelines and Outcomes. IndiGO is a clinical decision support tool designed for doctors and other care providers to use at the point of care with their patients. According to the Archimedes website, IndiGO calculates and displays the risk a patient has of adverse events – such as heart attacks, strokes, and onset of diabetes. IndiGO then suggests and prioritizes the medications and/or lifestyle interventions that have the greatest impact on reducing that risk.
Rishi Misra, Implementation Manager for Archimedes, was kind enough to spend some time with us to talk about IndiGO, how it works, and why it’s such a powerful tool for engaging a patient in decisions about their health care.
CTH Blog:
Why don’t you start by providing some background on Archimedes?
Rishi Misra:
Archimedes was founded by David Eddy, one of the pioneers in bringing evidence-based practices to medicine. David recognized that many medical decisions were not being made based on the best available evidence. He wanted to integrate a more evidenced-based approach of making medical decisions based on statistics and clinically validated data. Based on that need, he built what we call the Archimedes Model. The Archimedes Model and the data engine that powers it are the foundation from which the tools the company offers today are built.
Archimedes was established as a part of Kaiser Permanente, and in 2006 it was spun out as a Kaiser Innovation – an independent, for-profit entity.
CTH Blog:
In layman’s terms, what is IndiGO, and how is it used?
RM:
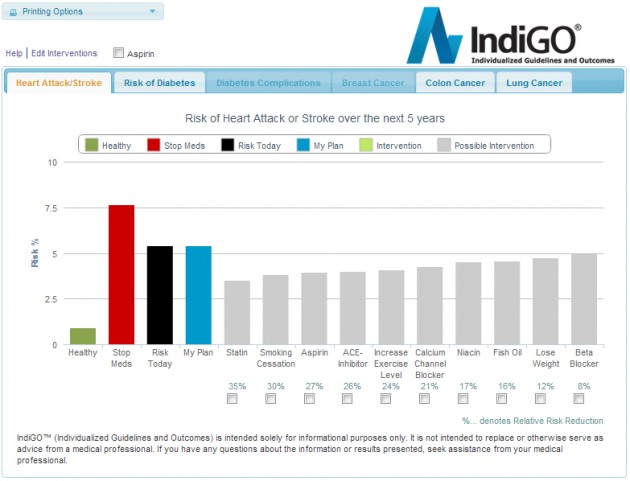
IndiGO is a clinical-decision support tool used to manage patient health at the point of care by showing patients what their risk is of certain adverse events on a five-year time horizon, and in some cases even over a lifetime. Based on the Archimedes Model, IndiGO provides suggested interventions to reduce a patient’s risk of heart attacks, strokes, and onset of diabetes.
CTH Blog:
How does it work? Does it use data from the electronic health record?
RM:
IndiGO incorporates 27 data elements from a patient’s EHR that are critical to computing the risk and suggested benefit of a particular intervention. The physician’s office or health care organization sends us de-identified patient data on a nightly basis, so we’re always looking at the latest, most current information. The data is then analyzed by the IndiGO engine, and results are returned to the submitting office. The risk assessment is very real-time, providing up-to-date information that the physicians have available to them.
CTH Blog:
And you use that data in the EHR to make these predictions?
RM:
Yes. Exactly. The IndiGO risk assessment shows how a patient’s decisions could reduce their health risk. It also illustrates how the risk could be magnified by their choice to ignore an intervention. For example, it might show that if they cease taking a medication, their risk could increase to, say, roughly seven times the risk of a healthy patient who is the same gender and age.
CTH Blog:
What is the response you are seeing from patients?
RM:
What we found is that this tool really serves as a trigger. Anecdotally, we know that physicians print out this screen and give it to their patients as a visual reinforcement of their conversation. The patients use the information in their risk assessment to activate them to adhere to the physician recommended intervention. We’ve heard of patients putting it up on their refrigerator as a reminder.
We’re doing a pilot with the Colorado Beacon Consortium, and we had patients come in and give testimonials. These were unscripted patients coming in to talk about how IndiGO has benefited the management of their personal health.
One patient – a retired engineer, 71 years old — said he never cared to go see his doctor. But once he saw IndiGO in action, he was hooked. He loved how it visually quantified his health. For him, this tool served as a differentiating factor, motivating him to see his doctor and stick with his plan. We find that IndiGO is not only helping physicians manage the health of their patients, it’s also serving as a distinguishing factor for patients to choose physicians using the tool, because they are provided with a more quantitative and more visual way of looking at their health. You can see how patients react to IndiGO in a video we have on YouTube.
CTH Blog:
A picture must really be worth a thousand words. What they see illustrated on the screen must resonate differently, because patients are told risk percentages all the time, but it doesn’t seem to have the same effect.
RM:
Right, because most risk percentages are an arbitrary number, and patients don’t know what it’s relative to. Whereas, with IndiGO, you might say, “Look, this is your current risk, and this is where a patient at the optimal level of health is.” And then you can show, visually, the effect their own actions can have on their health risks. That really motivates them. It’s powerful.
CTH Blog:
Is IndiGO used only for certain chronic conditions?
RM:
Yes, we focus on chronic conditions because of its significant impact on health and costs. Our results include risk of heart attack, stroke, diabetes, diabetes complications, and certain oncology-related models. We will soon be including a depression and COPD risk assessment module as well.
CTH Blog:
Do you customize this for customers?
RM:
We do. For example, thresholds can be configured based on the request of the client.
With Kaiser Permanente, it’s great, because they’ve put in a tremendous amount of resources into deploying KP HealthConnect [the organization’s electronic health record] and getting their EHR data to a point where IndiGO can be used for quality clinical analytics. There are many organizations that haven’t reached that point, though. With them, we serve as a tugboat to help organizations get to the point where they can use their data for quality clinical analytics.
The other thing we are doing with Kaiser Permanente is we’re working with kp.org [the Kaiser Permanente member site and portal to its personal health record, My Health Manager] to develop a version that members can use on their own. KP has 9 million members, and a lot of folks access their health information online. So we’re creating a user-friendly interface that will allow members to see their risk and how that’s changing over time in a very engaging way.
CTH Blog:
Is there a mobile version of IndiGO available?
RM:
There is an app that uses the tool as its risk engine. IndiGO was chosen by the Office of the National Coordinator and CDC for its Million Hearts Risk Check Challenge, where several app developers entered the competition by using our engine and the underlying model to develop apps. The winner — Marshfield Clinic Research Foundation’s “Heart Health Mobile” app — was announced in February, and it’s pretty cool. Patients can enter their information and basic parameters, and it gives them their risk profile based on what’s entered.
CTH Blog:
That’s terrific. Is this an app anyone can use, or only someone who is connected to a system that is already using Archimedes?
RM:
Anyone can do this. You can find it at the Apple App Store, and a web-based (HTML5) responsive design version is also available here.
CTH Blog:
Tell us about NCQA and the “GO Score.”
RM:
The GO (“Global Outcomes”) Score is being tested by NCQA to measure the proportion of adverse outcomes expected to be prevented in a population under current levels of care compared to a target level of care. It is potentially the first outcomes-based eMeasure. It’s in the process of being tested in leading organizations [including Kaiser Permanente] around the country.
CTH Blog:
What might be on the horizon for Archimedes?
RM:
Right now, a tool like the IndiGO model is built out for a population that is typically at high risk of heart attack, stroke, or diabetes. But I definitely think this can be extended to a younger population as well. And some of these gadgets that young people are using, like the Nike Fuel Band that helps manage their health, could really be interfaced with models like IndiGO that are clinically validated. We could show people on their mobile phones, for example, how the actions they are taking in their daily lives are affecting their health.