Total Health Blog | The future of health is here
Kaiser Permanente International Presents Cancer Care Reimagined
Last month, the Center for Total Health, in continued partnership with Kaiser Permanente International, hosted…
Kaiser Permanente International Customizes a Virtual Seminar for Dutch Startup Innovators
Hosted on the Center for Total Health’s virtual event platform, KP International recently presented…
Kaiser Permanente International Presents Population Health: Case Study in Diabetes and Hypertension Management
In collaboration with the Center for Total Health, Kaiser Permanente (KP) International launches a 5-part…
The Reginald F. Lewis Museum Recognizes African Americans in Health Care
During the last week of Black History Month, the Reginald F. Lewis Museum of African…
COVID-19 Vaccines and Communities of Color in Washington, DC
In support of the National African American Enrollment Week of Action, DC Health Link partnered…
Do the right thing – a Kaiser Permanente PSA on COVID-19
During our fight against COVID-19, we remain deeply committed to the health of our communities.…
Making masks to support our nonclinical personnel and guests
Find out how you can help in our fight against COVID-19 by making masks for…
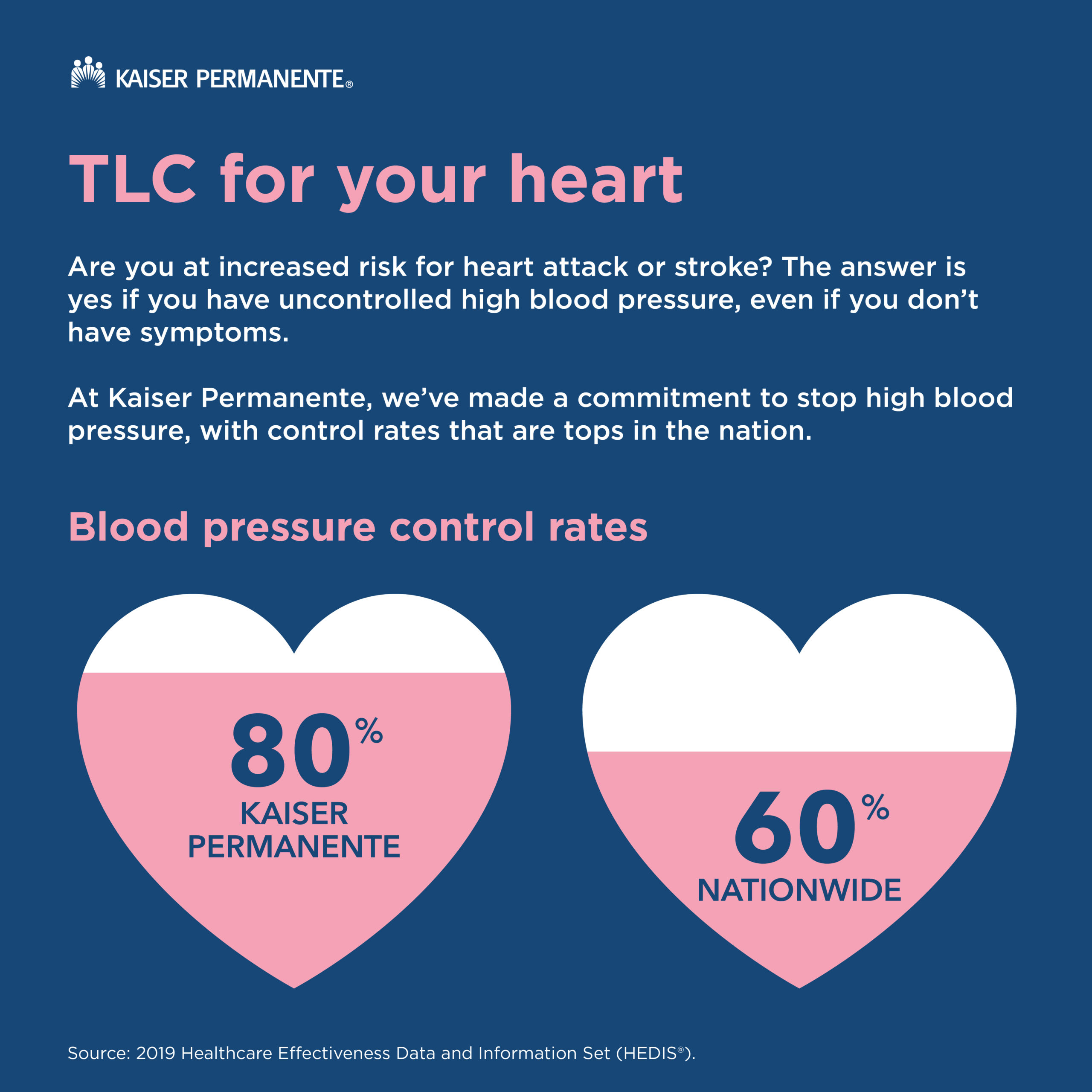
Take Prevention to Heart
Sorry to break it to you, but if you have uncontrolled blood pressure—you’re at a…
National Eating Disorders Awareness Week 2020
This year's theme for National Eating Disorders Awareness Week is "Come as You Are: Hindsight…
2019: A Big Year for the Center for Total Health!
Last year marked the Center for Total Health's 8th year as a dedicated space for…
National Efforts to Prevent Suicide
In late October, leaders from transportation, media, entertainment, law enforcement, technology, healthcare and other industries…
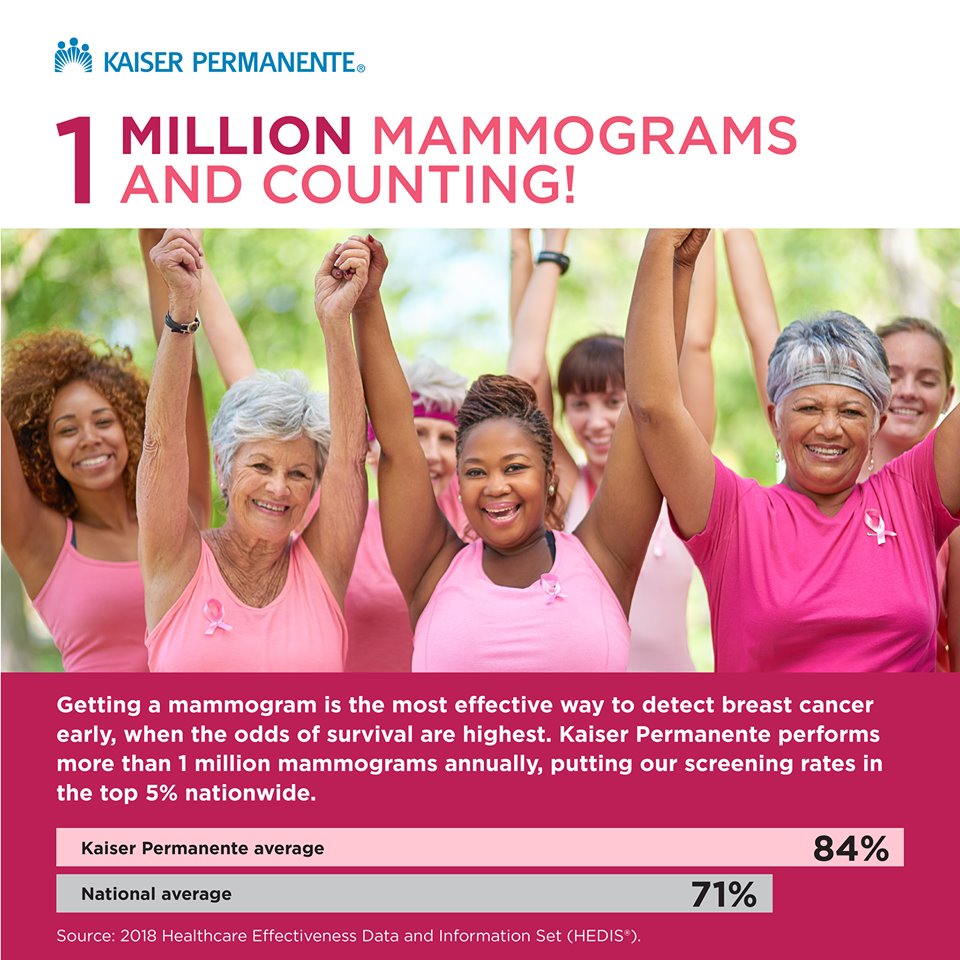
Less Anxiety, More Convenience for Breast Cancer Screening with Quick Mammogram Results
October is Breast Cancer Awareness Month, an annual campaign to raise awareness of the disease…
Generation Hope’s Two-Generation Solution to Poverty
A variety of innovative programs for healthier students or teachers have been featured at the…
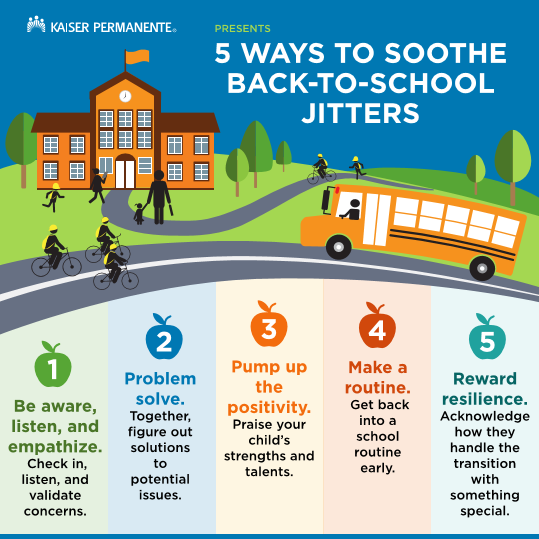
Five Tips for Reducing Back-to-School Anxiety
Mental preparation, with these five tips, for the transition back to school is as important…
August is National Breastfeeding Month
2019 marks the eighth year since the United States Breastfeeding Committee (USBC) marked August as…
Kaiser Permanente Recognizes and Addresses the Social Needs of Americans
A recent survey conducted by Kaiser Permanente (KP) finds that social needs—safe housing, balanced meals,…
Save the Drama for Trauma-Informed Care in Schools
Kaiser Permanente uses art to inspire school staff and teachers to rise above professional burnout…
Reducing Suicide Calls for Cross-Sector Collaboration
The National Action Alliance for Suicide Prevention (Action Alliance) works with more than 250 national…
Increasing Access to Birth Control Means More Than Just “The Pill”
More than half of all pregnancies, or nearly all teen pregnancies, in the United States…
How a Domestic Violence Survivor Strengthens Athletic Communities Against Abuse
Gridiron Terminal hosts its’ third summit—Not on My Turf: Strengthening Athletic Communities Against Abuse—at the…
Strengthening America’s Mental Health Workforce Together
With more than 44 million Americans having a diagnosable mental health condition—56 percent of which…
How can health systems intervene to prevent firearm death?
Firearm-related injuries account for tens of thousands of premature deaths of adults and children each…
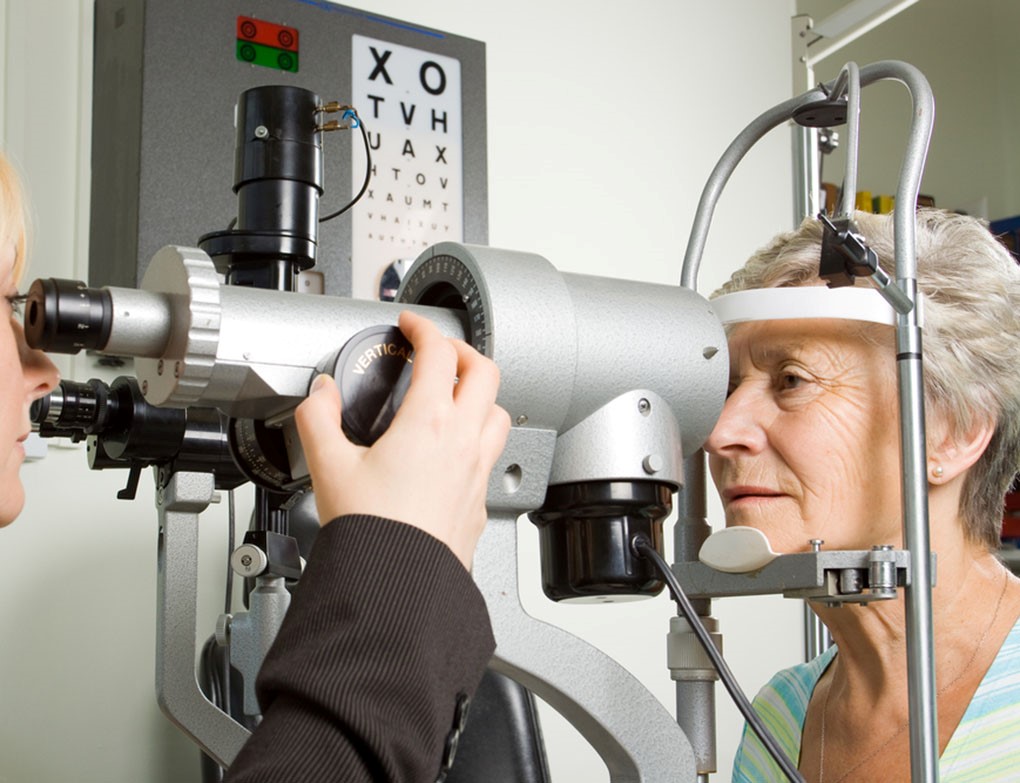
Common Vision Problems To Look Out For As You Age
As you age, it's not unusual to experience changes in vision, most often beginning around…
Healthy Aging – It’s never too late to start
It’s never too late to take your health in your hands and implement healthy practices…
Collaboration and Innovation Hold Promise for Cardiovascular Patients
Prioritizing patient needs topped the agenda at last month’s Value in Healthcare Initiative meeting, hosted…
Climate Change – An ‘Urgent’ Human Health Issue
Kaiser Permanente was the leading health care sponsor of the Global Climate Action Summit in…
Empowering the Next Generation of Potential KP Employees
Interns with the Kaiser Permanente’s Mid-Atlantic States Youth Internship Program recently closed the summer with a…
Honoring World Hepatitis Day
Worldwide, there are over 300 million people living with viral hepatitis, of which an estimated…
Kaiser Permanente Research Bank Improves Future of Health
The information carried within your DNA has the potential to change the future of health.…
The Center for a Mental Health & Wellness Tour
Now that July, National Minority Mental Health Month, is in full swing, the Center for…
U.S. Surgeon General Raises Awareness on Opioid Crisis
The Center for Total Health was honored with a recent visit from Dr. Jerome Adams,…
Center for Total Health Welcomes South Korean Government Officials
The Center for Total Health recently welcomed Gwanhoo Lee, the Professor of Information Technology and…
Kaiser Permanente and de Beaumont Foundation Work to Create Vibrant, Healthy Communities
WASHINGTON, D.C. – Kaiser Permanente, the nation’s largest integrated health system, has joined forces with…
Kaiser Permanente Researchers Develop New Models for Predicting Suicide Risk
SEATTLE — Combining data from electronic health records with results from standardized depression questionnaires better…
Kaiser Permanente Announces $200 Million Impact Investment, Partners with U.S. Mayors and CEOs to Address Housing Stability
OAKLAND, Calif. — Kaiser Permanente, the nation’s largest integrated health system, announced an impact investing…
Nurses Are Awesome
At the Center for Total Health, we think the world of nurses and the outstanding…
Celebrating America’s Nurses
Leaders, clinicians, advocates, scientists. These are just some of the roles that today’s nurses play.…
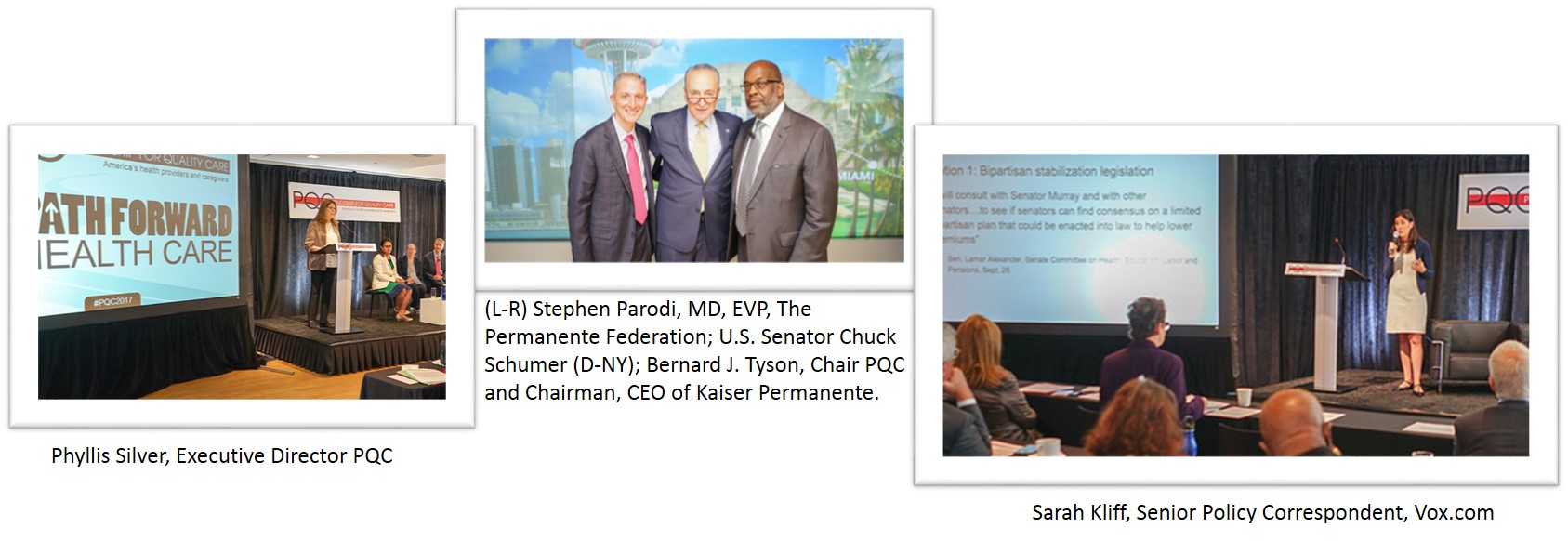
Reflections on High Drug Pricing in America: Where We Are and Where We’re Headed
Consider the following results from a recent Kaiser Family Foundation (KFF) poll on prescription drugs:…
April is Testicular Cancer Awareness Month
April is Testicular Cancer Awareness Month, and the Testicular Cancer Foundation wants to raise awareness for the most commonly…
Proud to Host National Action Alliance for Suicide Prevention
For the third year in a row, Kaiser Permanente hosted the National Action Alliance for…
Real-world Challenge Helps High School Students Explore Health Care Pathways
Solving for X may be the goal for a math test, but not a necessarily…
Solving Critical Issues for the Aging Population and Redefining the Aging Experience
Here at the Center for Total Health, life can sometimes be challenging for Leo and…
Patient-Based Simulation Education for Heart Failure Patients
Heart failure is a growing problem in the U.S., with over a million hospitalizations, skyrocketing…
Shattering Myths about Drug and Alcohol Abuse with Facts
Teenagers and young adults often receive a great deal of misinformation about drug and alcohol…
Staying on Track with New Year’s Resolutions
2018 is in full swing and that means we all are in the midst of…
It’s National Cervical Cancer Awareness Month
To bring some awareness of this important topic, we are sharing a recent Kaiser Permanente…
Telemedicine and a Vision for Health Care Without Walls
Consider these real-world vignettes: o A mother is in the midst of an emergency delivery…
Holiday Season Also Means It’s Flu Season
As the holidays are in full swing, the flu season, unfortunately, is also off to…
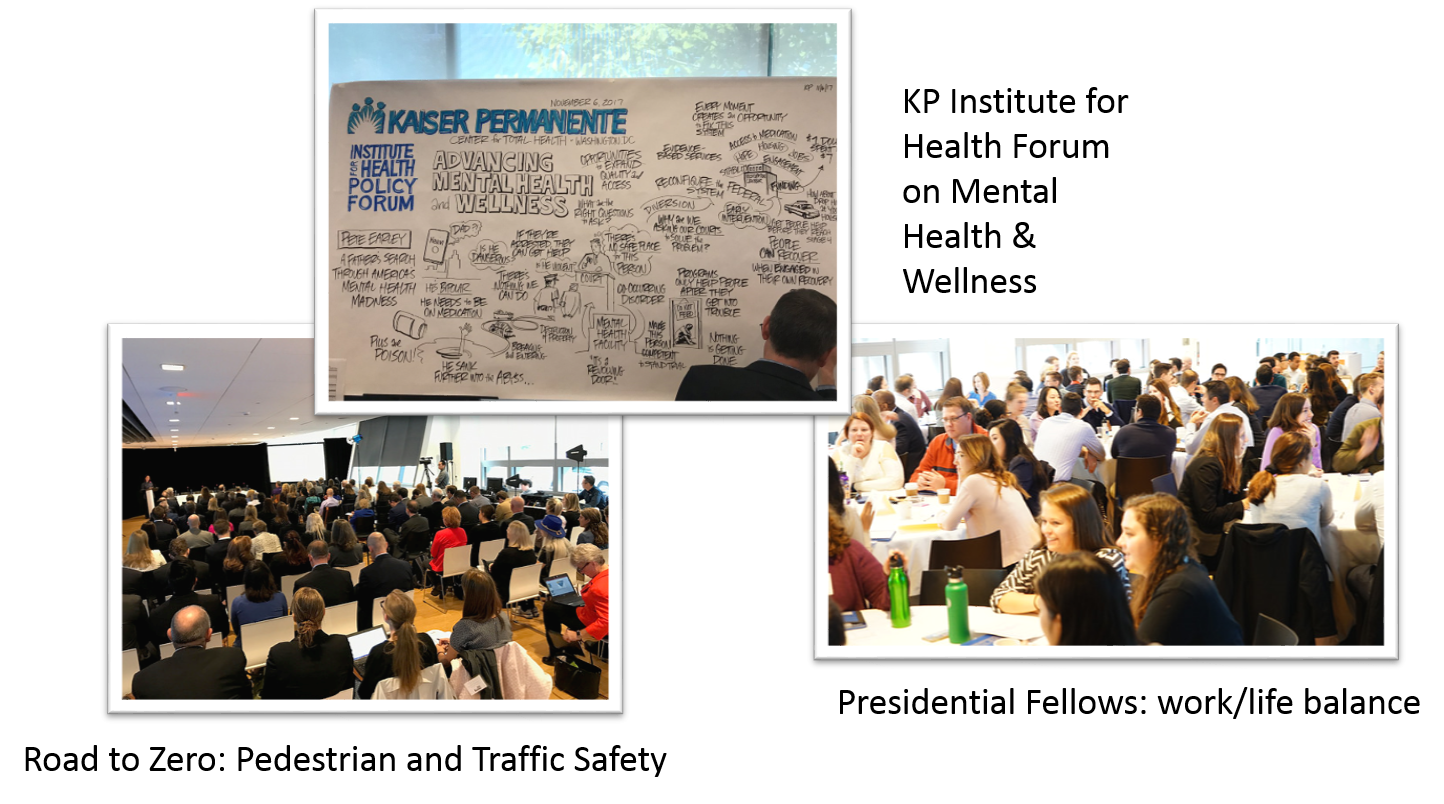
Hot Topics at the Center
A lot has happened recently at the Kaiser Permanente Center for Total Health, where we…
Patient Portals a Helping Hand for Families
A new study – designed with the direct assistance of Kaiser Permanente members who use…
November is National Alzheimer’s Disease Awareness Month
Currently, more than 5 million people in the United States are living with Alzheimer's disease.…
It was a great October at the Center!
Here’s what you missed at the Center for Total Health in October October was a…
Healthy Eating for a Healthy Meeting
Lunchtime often provides a crucial moment to refresh during a hectic workday, conference or meeting.…
BUILDing Together for Healthier Communities
Health is commonly thought of through the lens of health care–the doctor’s office, the emergency…
Here’s what you missed at the Center for Total Health in September
The status of your health extends far beyond the four walls of a medical center…
Center for Total Health Welcomes Workgroup on Measuring Wellbeing in Communities
On September 8, leaders in measurement development convened at Kaiser Permanente’s Center for Total Health…
Building Healthy Communities Requires All of Us
When multiple institutions across varying sectors work in alignment, we will create better health outcomes…
Defining the Next Generation of Behavioral Health Strategies
Today, one in five American adults experiences a mental health issue, and one in 10…
Kaiser Permanente Invites You to Thrive After 60
Earlier this year, Kaiser Permanente Mid-Atlantic hosted nearly 1,000 members and non-members for “Thriving After…
Physician researchers build bridges to health care innovation
A new joint program of The Permanente Medical Group and the Division of Research in…
The Importance of Immunizations as Kids Head Back to School
As the new school year approaches, pediatricians are reminding parents of the crucial role immunizations…
Celebrating Breastfeeding Awareness Initiatives at the Center for Total Health
During National Breastfeeding Month, Kaiser Permanente is highlighting the importance of breastfeeding as one component…
Walking Meetings: Taking Total Health Outdoors
“Total health is more than a visit to the doctor, and more than your medical…
Kaiser Permanente School of Medicine Will Care About Student Wellbeing
In 2019, Kaiser Permanente will be opening a Medical School located in Southern California. Currently,…
Kaiser Permanente Welcomes IADB Division of Social Protection and Health
Here at the Center, Kaiser Permanente International offers a forum for sharing Kaiser Permanente’s knowledge and experience…
National Action Alliance for Suicide Prevention
On June 20, the Center for Total Health welcomed the National Action Alliance for Suicide…
Steer Your Health Care Where You Want It to Go
Most people don’t hesitate to advocate for the kind of quality service they expect when…
What Skills and Supports Are Needed for Effective Practice in an Integrated Delivery System?
A new study published in INQUIRY: The Journal of Health Care Organization, Provision, and Financing…
Here’s What Happened in June at the Center
If you haven’t visited the Center for Total Health recently, June kicked off this summer…
National Collaborative on Education and Health
The National Collaborative on Education and Health steering committee met June 6 and 7 at…
IAEE Inaugural Evening Educational Event
The Kaiser Permanente Center for Total Health recently welcomed the D.C. Chapter of the International…
Create Your Life Care Plan Now
We all try to prepare for life’s major events but, if you suddenly became injured…
Join the Road to Zero Coalition
Recently, the Road to Zero coalition hosted “Saving Lives on our Roadways at the Merging Intersection…
Employees + Workforce Health = Increased Daily Productivity
Kaiser Permanente's Workforce Health team has geared up to offer their annual Mid-Atlantic Summer 2017…
The National Academy of Social Insurance Gala Was a Success!
Last week, the Kaiser Permanente Center for Total Health hosted and served as a sponsor of…
The Healthcare Anchor Network adds new members
This week, the Healthcare Anchor Network officially launched and expanded its membership to include: Adventist…
Here’s What Happened in May at the Center
If you haven't visited the Center for Total Health recently, May was a busy month…
Supporting Healthy Communities through Collaboration: The Healthcare Anchor Network
Supporting Healthy Communities through Collaboration: The Healthcare Anchor Network Last December, 40 health systems gathered…
The Center for Total Health hosts third-annual Better Together Health
On May 24, the Kaiser Permanente Center for Total Health hosted All Systems Go! Closing…
Violence and Your Health
The National Health Collaborative on Violence and Abuse (NHCVA), comprised of more than 30 national…